Prostatitis and Erectile Dysfunction: What’s the Connection?
Written by Dr. Deepali Anand

Dr. Deepali is a medical writer and healthcare professional with a background in clinical surgery and patient care. Having transitioned from active clinical practice to medical communications, she specializes in bridging the gap between complex clinical data and patient education. Dr. Deepali is dedicated to creating evidence-based content that is grounded in scientific rigor and empathy, ensuring that sensitive topics like sexual wellness and mental health are accessible and empowering for every reader.
•
September 9, 2025
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Quick Read
Yes, prostatitis can cause erectile dysfunction, research confirms that men with prostatitis are about three times more likely to experience ED. The link happens through inflammation affecting blood flow, nerve pathways, and hormones, plus the psychological stress of dealing with chronic pain and urinary symptoms creates a cycle that worsens both conditions. The encouraging news: this type of ED is usually completely reversible with proper treatment that addresses both the prostate inflammation and sexual function together. Most men see significant improvement within 6-8 weeks when treated early.Most men see dramatic improvement within 6-8 weeks using a comprehensive approach - antibiotics or anti-inflammatories for the prostatitis, PDE5 inhibitors like Cialis for blood flow, pelvic floor therapy for muscle tension, and stress management for the psychological component.
Prostatitis-erectile dysfunction: are they connected? The answer is yes. Prostatitis can contribute to erectile dysfunction through a mix of physical changes and psychological stress.
If you’ve been dealing with urinary issues, pelvic pain, or discomfort during sex and are now worried about your erections, you’re not alone. Research shows a strong link between prostatitis and ED, but the good news is that both are highly treatable.
In this article, we’ll explore how prostatitis affects sexual function, what the science says, and the treatments and lifestyle steps that can help you restore both your prostate health and your confidence.
What is Prostatitis?
Prostatitis simply means inflammation of the prostate gland. The prostate is a small but important part of the male reproductive system. Its main job is to produce prostate fluid, a key component of semen that helps nourish sperm and gives semen its white color.
Although prostatitis is more common in men over 50, it can affect men at any age. This raises an important question many men have: Can prostatitis cause erectile dysfunction? Let’s explore the connection.
Allo asks
What’s Your Biggest Concern with Prostatitis & ED?
Can Prostatitis Cause Erectile Dysfunction?
Yes, prostatitis can lead to erectile dysfunction. The connection comes from a mix of physical and psychological factors.
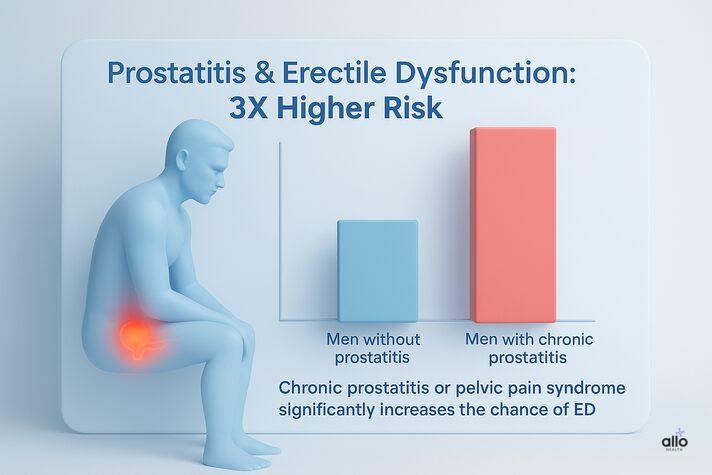
Research[1] shows a clear link between different types of prostatitis and ED, with erectile dysfunction being one of the most common complications men report. In fact, one study[2] found that men with chronic prostatitis or chronic pelvic pain syndrome are about three times more likely to experience ED compared to those without it.
Why does this happen? Chronic pain, ongoing lower urinary tract symptoms, and discomfort during ejaculation can all interfere with sexual activity. Over time, this not only affects the body but also creates stress, anxiety, and performance worries, together making erectile dysfunction more likely.
Types of Prostatitis and Their Link to Erectile Dysfunction
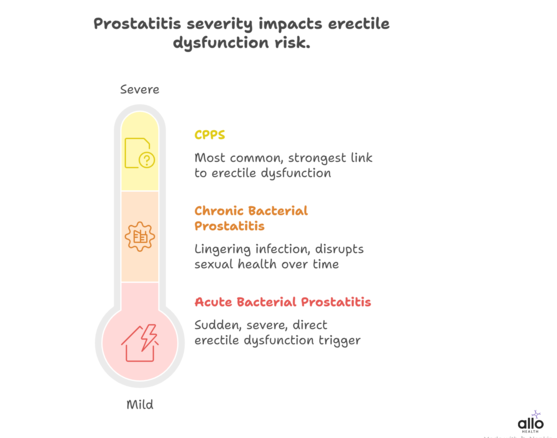
1. Acute Bacterial Prostatitis
This is the sudden, severe form of prostatitis. Because of the intense inflammation and pain, it can directly trigger erectile dysfunction, often making sexual activity very difficult until the infection is treated.
2. Chronic Bacterial Prostatitis
Here, the infection lingers. The result is ongoing inflammation that disrupts sexual health over time. Men often report persistent issues with erections and overall sexual satisfaction.[3]
3. Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CPPS)
This is by far the most common form, accounting for up to 90% of cases of prostatitis. It also has the strongest link to sexual dysfunction. Studies[4] suggest that 49-62% of men with CPPS experience erectile dysfunction, along with other issues like pain during or after sex.
How Can Prostatitis Cause Erectile Dysfunction
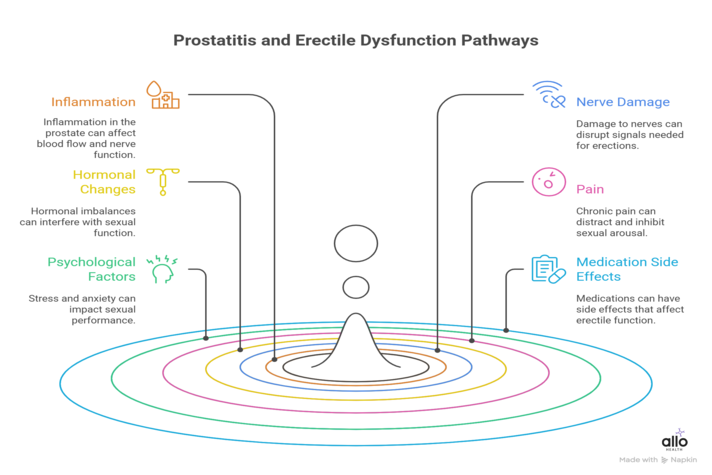
Prostatitis can affect erections in several ways, involving the body, mind, and even the treatments used. Here are the main pathways:
1. Inflammation and Vascular Effects
Chronic inflammation in prostatitis can damage blood vessels. Inflammatory molecules called cytokines interfere with the normal contraction and relaxation of penile muscles.
Research also shows that prostatitis can impair endothelial cells (the inner lining of blood vessels), reducing nitric oxide release, a key step in relaxing blood vessels for proper blood flow during erections.
2. Nerve Damage
Inflammation and pelvic pain may irritate or damage the nerve pathways (pelvic nerve irritation) that control erections. This disrupts both the physical signals and the psychological confidence needed for arousal.
This often creates a cycle where pain worsens sexual dysfunction and sexual dysfunction worsens anxiety.
3. Hormonal Changes
Ongoing inflammation can disrupt hormonal balance, including low testosterone levels, which are essential for healthy erectile function.[5]
4. Pain
Pelvic pain, especially during or after ejaculation, can create a mental barrier toward sexual activity. What should feel pleasurable becomes associated with discomfort, which in turn lowers both desire and performance.
5. Psychological Factors
Living with chronic prostatitis often brings stress, frustration, and anxiety. Due to concerns about sexual performance(performance anxiety), a cycle of anxiety and erectile problems can quickly develop.
6. Medication Side Effects
Some treatments for prostatitis, such as alpha-blockers (used to relax urinary flow in urinary tract infection), may occasionally affect erectile function as a side effect.
Does Treating Prostatitis Improve ED?
The good news: prostatitis-related erectile dysfunction is usually reversible. Once the inflammation is treated, sexual function often returns. Many men notice recovery within weeks; others take a few months. In most cases, improvement is expected, not rare.[6]
If ED continues, it needs separate care. Ongoing issues may stem from performance anxiety, stress, or underlying vascular problems.
Early treatment gives the best results. Tackling prostatitis quickly prevents long-term changes in nerves, blood flow, and confidence, making full recovery far more likely.
Prostatitis and erectile dysfunction often go hand in hand, but the good news is that with the right treatment, most men see real improvement in both.
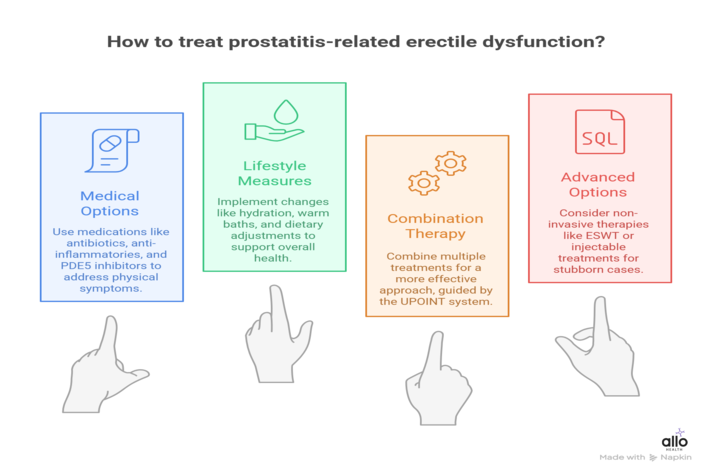
Prostatitis-Related Erectile Dysfunction Treatment
With the right treatment plan, most men see improvements in both prostatitis and erectile function. The key is early diagnosis, patience with the process, and a holistic approach that addresses both body and mind.
1. For Prostatitis
Antibiotics: Common options include fluoroquinolones, trimethoprim-sulfamethoxazole, or doxycycline, for 4–12 weeks.
Anti-inflammatories (ibuprofen, naproxen) calm swelling and reduce pain.
Alpha-blockers (tamsulosin, alfuzosin) relax the muscles around the prostate and bladder neck, like loosening a tight collar.[7]
Lifestyle measures that actually help:
Stay well-hydrated
Try warm sitz baths (15–20 minutes, 2–3 times a day).
Cut back on irritants like alcohol, caffeine, and spicy foods.
2. Addressing the ED Component
Medical options:
- PDE5 inhibitors (Viagra, Cialis, Levitra) improve blood flow while prostatitis heals.
- Daily low-dose tadalafil (5 mg) is often a good choice because it helps with both urinary symptoms and erectile function.
- Pain management medications may be needed if discomfort interferes with intimacy.
Beyond pills:
- Pelvic floor therapy: Chronic inflammation can make these muscles tight, and pelvic floor therapy can help restore balance.
- Counseling or sex therapy: Because the mental side of sexual health is just as important as the physical.
- Stress management: Relaxation techniques, mindfulness, or exercise can make a huge difference.
3. Combination Therapy
Research shows that using a combination of treatments works better than relying on a single medicine. Doctors often follow the UPOINT system[8] (Urinary, Psychosocial, Organ-specific, Infection, Neurological, Tenderness) to guide a tailored plan.
Common combinations include:
- Alpha-blockers (like tamsulosin, alfuzosin) to ease urinary symptoms
- Anti-inflammatories (including natural options like quercetin)
- Antibiotics are used when an infection is present
- Herbal extracts (saw palmetto, lycopene, selenium)
- PDE5 inhibitors to improve erections
4. Advanced Options (For Stubborn Cases)
- Extracorporeal Shock Wave Therapy (ESWT): Despite the intimidating name, it’s non-invasive and has shown 70–80% improvement rates in men with ED.[9]
- Specialized pain therapies for chronic pelvic pain syndromes.
- Injectable ED treatments if oral medications aren’t enough.
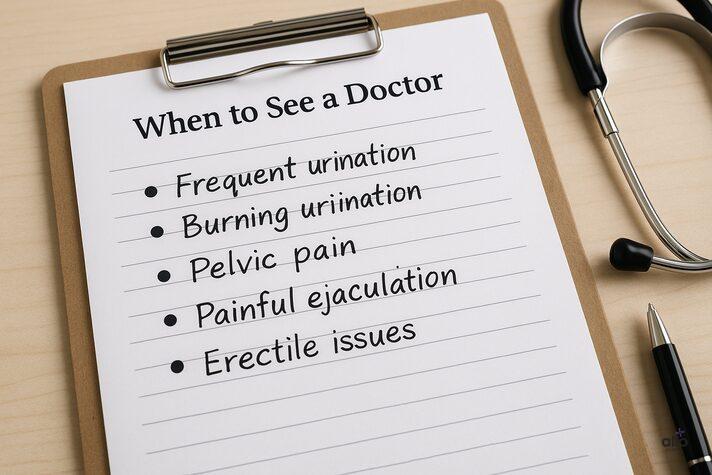
When to See a Doctor
Your body often gives clear signals when the prostate isn’t happy. Watch for common symptoms of prostatitis:
- Frequent urination, needing to pee every hour, or waking up multiple times at night.
- Burning sensation while urinating.
- Pelvic pain, dull ache, pressure, or sharp discomfort in the lower abdomen, perineum (between scrotum and anus), or lower back.
- Painful ejaculation
If you notice ED along with urinary or pelvic symptoms, that’s your cue to seek help right away. Don’t wait it out; early treatment greatly improves your chances of full recovery.
Bottom Line
Prostatitis and erectile dysfunction are closely linked, but both are highly treatable. The sooner you seek care, the better your chances of full recovery. A comprehensive approach that addresses prostate health, sexual function, and overall well-being together gives men the best shot at restoring confidence and quality of life.
Disclaimer
The following blog article provides general information and insights on various topics. However, it is important to note that the information presented is not intended as professional advice in any specific field or area. The content of this blog is for general educational and informational purposes only. The content should not be interpreted as endorsement, recommendation, or guarantee of any product, service, or information mentioned. Readers are solely responsible for the decisions and actions they take based on the information provided in this blog. It is essential to exercise individual judgment, critical thinking, and personal responsibility when applying or implementing any information or suggestions discussed in the blog.
Most Asked Questions
Will prostatitis cause erectile dysfunction?
Not always, but prostatitis can increase the risk of ED. Inflammation, pain, and stress from prostatitis can interfere with erections. The good news is that when prostatitis is treated, sexual function often improves as well.
Can prostatitis be reversed?
Yes. With the right treatment like antibiotics (if bacterial), anti-inflammatories, and lifestyle changes, prostatitis symptoms can be managed or even completely resolved. Chronic prostatitis may take longer, but significant relief is still possible.
What are the common symptoms of prostatitis?
Frequent urination (especially at night), burning during urination, pelvic or lower back pain, painful ejaculation, and sometimes erectile difficulties. Not everyone has all the symptoms, but any combination is worth discussing with a doctor.
How do you treat erectile dysfunction caused by prostatitis?
The first step is treating the prostatitis itself. Alongside that, ED can be managed with medications like PDE5 inhibitors (Viagra, Cialis), pelvic floor therapy, counseling, and stress management. Treating both together usually brings the best results.
Is prostatitis-related erectile dysfunction permanent?
In most cases, no. Once prostatitis is under control, erections often return to normal. If ED lingers, it may be due to anxiety, stress, or other health factors, which can be treated separately.
Sources
- 1.
Prevalence of Sexual Dysfunction with Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS): An Updated Systematic Review and Meta-Analysis
- 2.
Erectile Dysfunction in Chronic Prostatitis/Chronic Pelvic Pain Syndrome: Outcomes from a Multi-Center Study and Risk Factor Analysis in a Single Center
- 3.
Prostatic Disease and Sexual Dysfunction
- 4.
Prevalence of Sexual Dysfunction with Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS): An Updated Systematic Review and Meta-Analysis
- 5.
Study on the relationship between sex hormone changes and erectile dysfunction in patients with chronic prostatitis/chronic pelvic pain syndrome
- 6.
The Effect of Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS) on Erectile Function: A Systematic Review and Meta-Analysis
- 7.
Prostatitis in Men: Causes, Symptoms, Diagnosis & Treatment
- 8.
Erectile Dysfunction in Chronic Prostatitis/Chronic Pelvic Pain Syndrome: Outcomes from a Multi-Center Study and Risk Factor Analysis in a Single Center
- 9.
Extracorporeal Shockwave Therapy (ESWT) Alleviates Pain, Enhances Erectile Function and Improves Quality of Life in Patients with Chronic Prostatitis/Chronic Pelvic Pain Syndrome


